Chagas disease:
a health concern in the United States
Chagas disease may not be widely recognized in the United States
Chagas disease (American trypanosomiasis) is an infectious tropical disease caused by single-cell parasites called Trypanosoma cruzi (T. cruzi), which are transmitted by triatomines or “kissing bugs.”1
Endemic throughout much of Latin America, Chagas disease is also a health concern in the United States, where it affects an estimated 300,000 people.2,3 In fact, cases in the United States account for approximately 75% of the total in nonendemic countries worldwide.1
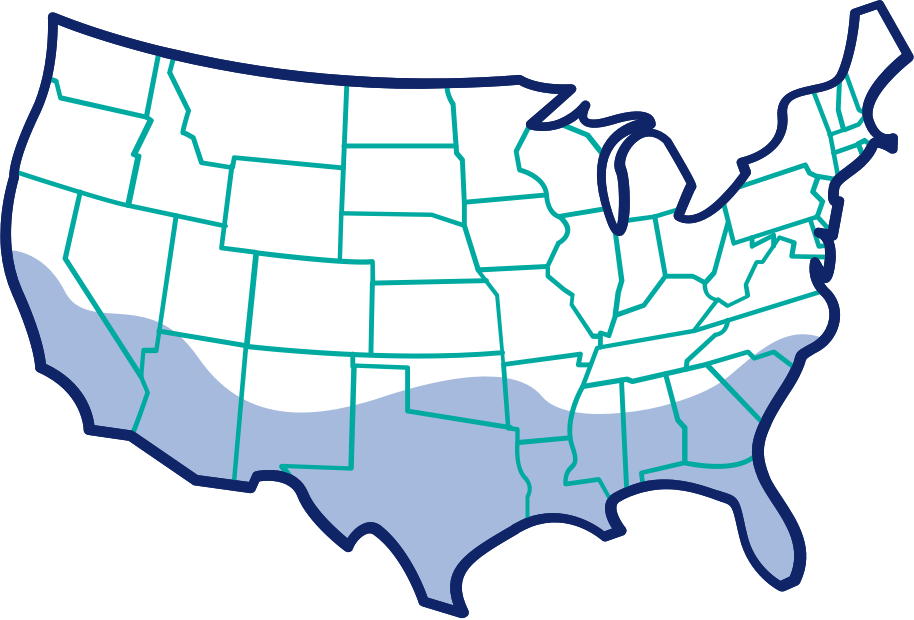
Although most cases of Chagas disease in the United States originated in Central or South America, triatomines are native to the southern United States.1

Chagas disease is primarily spread in countries where it is endemic
Chagas disease is transmitted to humans via the feces of infected triatomines, which ingest T. cruzi when feeding on blood of infected hosts and carry the parasites in their digestive tracts.2-4 When biting a human, they defecate, and the parasites in the feces enter the body through the bite wound and mucous membranes, such as the conjunctivae.4
Chagas disease can also be transmitted from an infected mother to her unborn child.5 Rarer forms of transmission include organ transplantation, blood transfusion, and ingestion of contaminated food.2,3
Chagas disease: a hidden infection that can lead to major complications
Chagas disease is considered a “neglected” tropical disease. In 2010, the FDA launched a program to support the diagnosis, treatment, and prevention of neglected tropical diseases, including Chagas disease.6
Chagas disease is severely underdiagnosed, and less than 1% of infected individuals receive treatment.7,8 This is in part because patients exhibit a wide range of nonspecific symptoms or no symptoms at all.3
Chagas disease occurs in 2 phases: an early (acute) phase shortly after a patient is infected with the parasite, and a chronic phase that persists for years.3 Each phase has different sets of symptoms and presentations.3,4
Acute Phase3
- Lasts from a few weeks to 2-3 months
- Patients may experience mild and nonspecific symptoms, such as:
- Fever
- Body aches
- Tiredness
- Swelling around the site of entry
Chronic Phase3
- Can persist for years and may lead to:
- Cardiovascular (CV) problems
- Gastrointestinal (GI) tract problems
- Patients with immune disorders, such as human immunodeficiency virus (HIV), or organ transplant are at higher risk for developing more severe disease
CV and GI complications in the chronic phase can be serious and potentially life threatening

Potential CV complications4,5:
- Heart rhythm disturbances
- Cardiomyopathy
- Congestive heart failure
- Thromboembolism

Potential GI complications4,5:
- Megaesophagus
- Megacolon
- Acute obstruction
Of the estimated 300,000 cases in the United States, 30,000-45,000 individuals are likely to have undiagnosed cardiomyopathy associated with the disease.9
Congenital infection has its own set of nonspecific and potentially serious complications
About 10%-40% of congenitally infected infants can present with prematurity, hepatosplenomegaly, jaundice, anemia, and thrombocytopenia.4
Mortality among infected infants is significantly higher than in uninfected infants, ranging from <5%-20%.10
Recognizing risks and adequate testing are key to timely diagnosis of Chagas disease
Risk factors for contracting Chagas disease in endemic areas include triatomine exposure, blood transfusion, organ transplantation, being born to an infected mother, and rarely, through consumption of infected food or laboratory accidents.2,11
Patients who have kissing bugs in their environment may be at risk.11
Recommended diagnostic tests

In the acute phase:
Definitive diagnosis of acute infection is made using various techniques when parasites are detected in the bloodstream. If organisms are not detected, but risk factors or symptoms suggest infection, polymerase chain reaction (PCR) tests may be used to confirm diagnosis.3,5

In the chronic phase:
Chagas disease is usually diagnosed with tests to detect antigen-specific immunoglobulin G (IgG) antibodies. Although available tests have good sensitivity, false positives may occur in patients with autoimmune diseases or other infections. Thus, 2 different tests are recommended to confirm diagnosis.5
Who should be treated?
After confirmed diagnosis, treatment for Chagas disease is recommended for all of the following4,12:
- Pediatric patients with acute disease
- Infants with congenital infection weighing at least 2.5 kg
- Children aged younger than 18 years, with positive enzyme-linked immunosorbent assay (ELISA) results
Early treatment is important in children with acute disease and in newborns with congenital disease.4 Chagas disease may evolve into a lifelong chronic infection. Up to 30% of chronically infected patients may experience life-threatening CV and/or GI complications.4



